
Osteoporosis is a
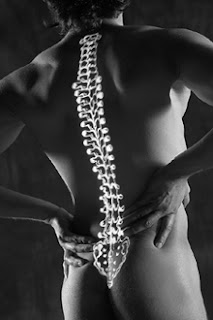
skeletal disorder characterized by compromised bone strength, which predisposes
to increased risk of fractures. Contrary to other common diseases that produce distinct
symptoms, osteoporosis can exist undetected for a longtime before complications
like bone fractures, height loss and bending of spinal column occur.
A woman left untreated
is predicted to have a 50% chance of suffering from an osteoporotic fracture
sometime in her life. In addition to spinal fractures, common fracture
locations include the wrist (hand), ankles (foot),and hip. Thus, it is
important that physicians and patients take measures to prevent and treat the
disease.
Bone is in a constant
state of turnover or activity throughout life. The basic pathology in
osteoporosis is an imbalance between bone resorption and bone formation. The
most common cause of this imbalance is menopause (stop of periods).The peak
bone mass is reached, at the age of 20 to 30 years.
After peak bone mass is
reached, the bone remodeling process is in a state of equilibrium until
menopause. Stop of menstrual period sleads to rapid bone loss of approximately
to half of the total spinal bone mass.
This is then followed
by a slower rate of bone loss(0.5%/year), which is related to aging due to
decrease in physical activity and there are other secondary cause for osteoporosis.
Various techniques are
available to quantify bone mass, but the most accurate and precise is the
central dual-energy x-ray absorptiometry (DXA) scan. A strong correlation
exists between fracture risk and bone density.
The World Health
Organization (WHO) criteria are the widely accepted basis for osteoporosis diagnosis.
Osteoporosis was defined as a T-score equal to or less than -2.5. T-scores
above this cutoff but below -1.0 define osteopenia, or low bone mass. Normal
BMD is 1 SD above or below the mean (T-score of -1 to +1). An individual who
has a T-score of -2.5 or less and has suffered from an osteoporotic fracture is
considered to have severe or established osteoporosis. Clinicians therefore,
incorporate Bone Mineral Density (BMD), age, and prior fracture in their
assessment of fracture risk and patient management to improve their bone
health.
Successful treatment of
osteoporosis requires a careful choice of blood and urine tests to determine
the presence of secondary causes of osteoporosis like liver, kidney, bowel
disease, hormone imbalance and cancer.
Osteoporosis therapies
are designed to improve bone strength and reduce the risk for fracture.
Treatment of osteoporosis is with drugs which can be taken by mouth (daily or
monthly) or once in a year if given intravenously through blood. Drugs for osteoporosis
can be divided into two major classes: anti-resorptive and anabolic agents.
Within a few weeks of starting therapy, patients
will usually report an improvement in clinical symptoms like alleviation of
bone pain, improvement in muscle strength, and possibly increased sense of
well-being.
Greater decrease in
blood and urine markers of bone resorption and increase in bone strength after
initiation of treatment. Thus it is possible to predict a reduction in fracture
risk in response to therapy within months of initiation of treatment.
There may be an improvement
in Bone Mineral Density (BMD) in the spine and hip even within just 1 year of
treatment. All patients should be counseled on exercises. The benefits of
exercise include improved muscle strength, gait, and balance, and better sense
of well-being.
Here, the concept is
that if Bone Mineral Density (BMD) continues to decline over the patient
lifetime, the risk for fracture is greater as the patient gets older. Thus
earlier intervention reduces the lifetime risk of fracture.













No comments:
Post a Comment